Stereotactic Spine Radiosurgery
Stereotactic spine radiation surgery (SRS) is a noninvasive and precisely targeted treatment for spinal tumors.
What is stereotactic spinal radiosurgery?
SRS is a noninvasive, innovative treatment for malignant or benign spine tumors.
Spine tumors may develop in the spinal column's nerves, bones, or other tissues. These tumors can be benign, slow-growing cancerous tumors, or aggressive high-grade tumors. Metastatic spine tumors account for more than 90% of all spinal tumors. They can cause painful symptoms and require invasive treatments.
Stereotactic radiosurgery for the spine can relieve pain using a nonsurgical, noninvasive procedure. The radiation is delivered precisely to the tumor using a 3-dimensional targeting system. This is the most common treatment for spine tumors and can be part of a comprehensive treatment plan.
Advertisement
Cleveland Clinic is an academic medical center that operates on a non-profit basis. Advertisement on our website helps us support our mission. We do not recommend products or services that are not from Cleveland Clinic. Policy
What are the possible effects of spinal tumors?
Untreated spine tumors may destroy spine bones, resulting in a loss of spinal column stability and sometimes compression of the spinal cord or nerves. It can lead to paralysis, nerve damage, or spinal cord injury.
A new treatment option
Spinal tumors can have serious consequences if not treated early. Traditional options beyond analgesics include surgery, conventional radiotherapy over days or weeks, and chemotherapy. Stereotactic radiosurgery is a treatment that can be used alone or with other treatments to treat spine tumors.
Procedure Details
What is stereotactic radiosurgery?
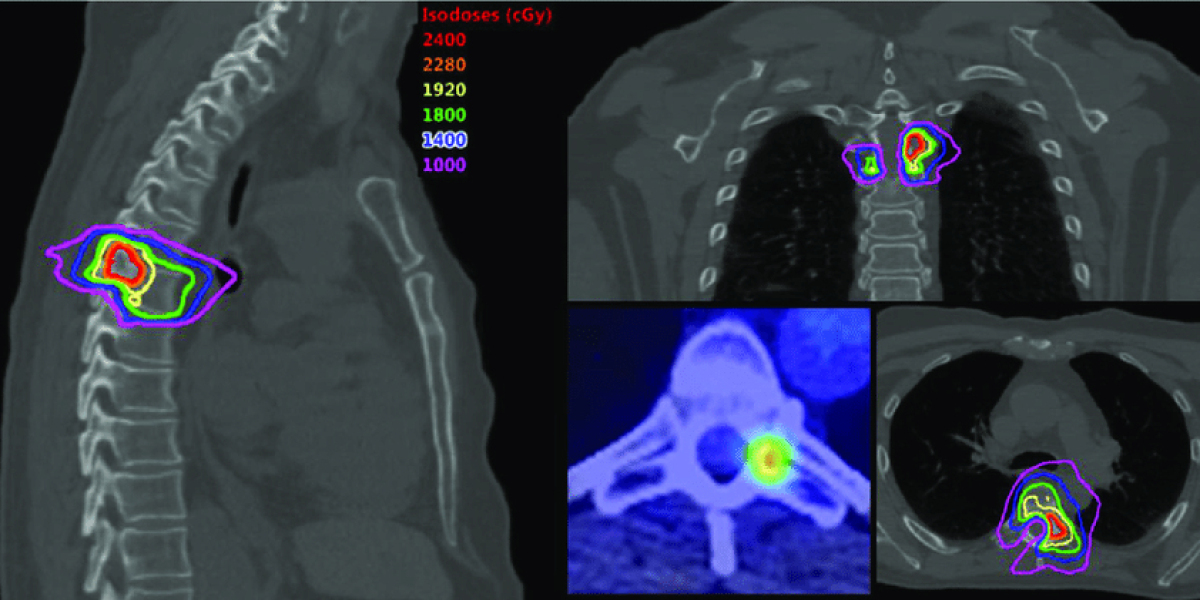
Stereotactic spinal radiosurgery is a technique that uses high-dose radiation to treat the tumor. SRS uses narrow radiation beams to target the tumor precisely, maximizing the radiation dose while minimizing the exposure to normal tissue. This highly targeted radiation dose can often result in pain relief or tumor reduction. One session of treatment on an outpatient basis is all that's required.
Advertisement
What happens after stereotactic spinal radiosurgery?
After stereotactic spinal radiosurgery, a neurosurgeon or radiation oncologist will schedule an MRI scan and a follow-up appointment. Depending on your condition, you may need to attend regular follow-up visits and undergo imaging studies.
What is the typical outcome of stereotactic spinal radiosurgery?
Success rates vary depending on the type and location of tumors being treated. Patients can expect to experience a local pain reduction of 85 to 90% within a month or less. Local tumor growth rates usually range between 80 to 90 percent.
Risks / Benefits
What are the benefits of stereotactic spinal radiosurgery (SRS)?
The recovery period is minimal. This procedure can often result in rapid pain relief and significantly improved functionality.
The stereotactic spine radiosurgery is used to:
- Pain relief
- The first line of treatment for spinal tumors
- Treatment of residual tumors after surgery
- Recurrence of tumor after conventional treatment
- When other treatments are not working, there is an alternative option.
Endometriosis: Understanding your pain relief options
Chronic pain is the main symptom. Pain is usually more intense during menstruation and ovulation.
These symptoms can include cramping, urination, bowel discomfort, and pain and tightness in the pelvic floor muscles. These symptoms can also interfere with daily life.
Endometriosis is not curable, but some treatments can help. Treatments vary in their effectiveness from person to person. The goal is to reduce or eliminate the pain caused by the condition. Continue reading to find out more about the specific treatments that can help.
Pain relief medications
Endometriosis can be treated with both prescription and non-prescription pain relievers. Many women with moderate to severe cases of endometriosis find that the over-the-counter pain relievers don't work well enough. Talk to your doctor for the best option based on your symptoms.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) are the most commonly prescribed pain medication for endometriosis. Ibuprofen and aspirin are available over-the-counter. There are also prescription NSAIDs available.
NSAIDs block the production of prostaglandins in your body, which is a biological compound. The prostaglandins are responsible for the swelling and inflammation that many women with endometriosis feel during their period.
What's the catch? The catch?
Take NSAIDs at least 48 to 72 hours before your first period and 24 to 48 before you begin ovulating. This gives the medication enough time to stop the production of prostaglandins. Your doctor may recommend taking pain medications for the week before your period if your cycle is unpredictable or irregular.
Not all medications work for everyone. Your doctor may advise you to try a different NSAID or NSAID in combination with other treatments. Some NSAIDs should not be taken with other medications. Talk to your doctor about any new medications you are considering taking.
Hormone Therapy
The pain caused by endometriosis can be treated with hormone therapy. This is done by controlling the hormonal fluctuations during your period. It can reduce or even stop menstruation. This is not a good option if you are trying to get pregnant.
Endometriosis is usually worsened by the hormones released around ovulation or your period. This can cause scarring to develop in the pelvis or thicken existing scarring. Hormone therapy aims to reduce scarring and prevent additional scarring.
Endometriosis can be treated with hormonal treatment.
Hormonal contraception
Since the 1950s, endometriosis has been treated with a combination of birth control pills. These pills are considered to be a staple of treatment. Many doctors also prescribe other forms of birth control, such as the hormonal IUD or vaginal rings.
Your doctor may suggest you take the pill continuously if you choose an oral contraceptive. You'll be able to avoid your period and the associated pain. You can skip your period for a few months (or years).
Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists
Gn-RH is a hormone that artificially induces menopause. It lowers estrogen levels and stops menstruation and ovulation. This can, in turn, help thin endometrial bruising.
GnRH agonists or antagonists are effective but can cause serious side effects in menopause, including vaginal dryness and hot flashes. These medications can be taken as a daily pill, a nasal spray, or an injection.
Progestin therapy
Progestins are believed to reduce endometriosis symptoms by slowing the endometrial scarring. Your gynecologist might recommend a progestin injection, pill, or IUD to manage your symptoms.
Hormonal therapies can reduce endometriosis pain and symptoms. It's important to remember that symptoms can return if your hormonal treatment is stopped at any point.
Surgery
Endometriosis is treated by surgery. The endometrial tumors that cause pain are removed. There are different types of surgery. The Endometriosis Foundation of America believes that laparoscopic surgery is the best treatment for endometriosis.
Laparoscopic surgery can be described as "conservative" because the goal is to remove endometrial tumors while maintaining healthy tissue.
A 2016 review published in Women's Health noted that surgery may be an effective way to reduce the pain associated with endometriosis. In a 2018 BMJ study, laparoscopic surgery effectively treated pelvic pain and bowel symptoms. It also improved women's quality of life who have endometriosis. The BMJ study involved more than 4,000 participants from several medical centers.
In the past, more invasive surgery was performed. In the past, endometriosis was treated with a hysterectomy and an oophorectomy (which removes the uterus, ovaries, and ovaries). These are not recommended to most people. Endometrial cancer can occur in other organs even if the uterus or ovaries have been removed.
Remember that surgery does not guarantee long-term pain relief. After the surgery, endometrial lesions and the pain that they cause may return.
Alternative and Complementary Therapies
Finding the right endometriosis treatment can take a lot of trial and error. You can combine your medical treatment with alternative and homeopathic remedies. Talk to your doctor first before trying any new therapies.
Alternative treatments for endometriosis may include:
- Acupuncture. The research on the treatment of endometriosis with acupuncture is limited. According to a 2017 review, acupuncture may help relieve endometriosis-related pain.
- Transcutaneous Electrical Nerve Stimulation (TENS) Machines. The TENS machines emit a low-level electrical current, which reduces pain and relaxes the muscles. A small research showed that TENS machines are highly effective at reducing pain.
- Heat. Warm baths and heating pads may help relax tight muscles and relieve pain associated with endometriosis.
- Stress Relief Chronic inflammation is associated with stress and can affect hormone levels. Meditation, yoga, coloring, and exercise are all stress management techniques.
Takeaway
Endometriosis is a painful condition. To manage your symptoms, trying different pain relief methods and finding out what works for you is important. Speak to your doctor and ask about the options available. Also, find out if they have any other treatments that may help.